The notorious 1918 influenza pandemic has received considerable attention amongst global historians. Crosby, Barry and Nicholson et al have written extensively on the history of pandemics.[1] They have provided important insights into the rates of morbidity and mortality caused by the pandemic, how individuals and groups responded to the pandemic, and the social, economic and public health consequences of the pandemic. However, their substantial contribution is largely limited to North America and Europe. Historical accounts on this topic in Africa is generally limited. Notable scholars argue that there is a significant absence of scholarly work on the nature and impact of the pandemic influenza in Africa.[2] This perceived lack of the African history on the 1918 pandemic influenza has compelled these scholars to inappropriately extrapolate part of global historical accounts to Africa, both retrospectively and prospectively. For example, Murray and colleagues used vital registry data across the world to estimate potential global pandemic influenza mortality but deliberatively excluded African mortality data from the global estimates.[3]Moreover, they still maintained that one third of the global 1918 influenza pandemic deaths occurred within sub-Saharan Africa. Relatedly, pandemic experts and observers often use analyses of the 1918 influenza pandemic in the Global North to make pessimistic statements about Africa’s future on the disease.[4] For example, there are claims that in an event there is a pandemic influenza outbreak “Africa will be worse attacked”[5] or since “Africa is already a distressed region with the most burden of diseases, its experiences and challenges due to effects of influenza will be more profound.”[6]’[7]
One common reason given for the absence of historical accounts of the pandemic in Africa is the lack of existing data.[8]And yet there is considerable quality data on the history of influenza in Africa stored at national archives awaiting to provide comprehensive analyses of the past. For example, official and unofficial records of the pandemic from Francophone, Lusophone and Anglophone countries in Africa exist in both national and colonial records. For the African colonies of Great Britain, vital registration data are immediately accessible from archival resources, both in published annual medical department reports and missionary medical reports, and in the correspondence files of the Colonial Offices (CO). These include records held in the Public Records Office (PRO) at the National Archives in Kew, England and various British colonies, which include entry books, gazettes, sessional papers and original correspondences such as dispatches between the colonial governor’s office and authorities in London, and letters from other government departments. In addition, various newspaper reports provide contemporary accounts that allow us to establish the social history of the pandemic outbreak in different colonial settings. These sources amongst others including key articles by Patterson, Pyle and others[9] on African perspectives of pandemic influenza remain an untapped resources for better understanding the nature and impact of the pandemic in Africa.
Drawing on these sources, in this article I focus on the colony of Nyasaland, now Malawi, located in southeast Africa and explore how the 1918 influenza disease spread, the rates of morbidity and mortality it produced, and the manner in which colonial administrators and local people responded to the pandemic. As such this paper seeks to speak to the current geographic bias characterizing analyses in this area by providing insights into how the pandemic played out in one particular African setting. Looking critically at how people responded to the pandemic, this paper also seeks to shed light on important lessons that can inform contemporary policy thinking on pandemic preparedness in the region.
First World War and Epidemics
During the First World War, Nyasaland was under the British rule and was a vital link in the East Africa campaign because of its strategic and military position; it allowed British troops to invade German East Africa (present day Tanzania) from its southern borders. The battle at Mlangali took place on 24 July 1916, when the First Battalion of the King’s Africa Rifles, a unit primarily made up of Malawians but led by British asilikali(soldiers), forced the Germans to retreat.[10]Despite triumph, the chief concern for the British was when, how and where the Germans would attack Nyasaland in retaliation. Given the importance of the battle, and lingering concerns about where the Germans would attack next, Nyasaland established defensive posts in several parts of the country. New lines of communication for fighting the enemy effectively were established. According to the Principal Medical Officer, H. Hearsey, new movement of the enemy in the direction south to north necessitated the Nyasa-Rhodesian Field Force to station along the entire eastern portion of Nyasaland and of Lake Nyasa.[11] These efforts substantially increased military movements and transportation demands for military hardware. Due to the lack of automobiles during the war, human porterage often referred to as Mtengatenga was used to transport goods, colonial masters and their followers from the south to north or vice visa, largely along the eastern shores of Lake Nyasa (Lake Malawi).[12] At the same time, there was massive recruitment of new young soldiers amid fears of a shortage of soldiers to maintain military dominance over the Germans.[13]
Nevertheless, continuous movement of troops, human carriers and their followers were of concern to public health professionals and doctors, with disease spread mapping their routes; this was especially so as epidemics such as smallpox and bubonic plague ravaged the country from 1915-1918.[14] In his report to the Chief Medical Officer in London, the Principal Medical Officer of Nyasaland, H. Hearsey, noted that the health of the Protectorate was not satisfactory owing to the extensive movement of military and local people, into and within the Protectorate, necessitated by military operations.[15] It was difficult to restrict the movement of soldiers so to check the spread of the disease, as the increasing military demands for labour had to be met.[16]In an excerpt taken from confidential correspondence from the Governor of Nyasaland to the Secretary of State, Governor Sir George Smith wrote: “while the war continues with its enormous drain on the medical profession generally, it is improbable to make changes within the medical service that divert this cause.”[17]Halting the war operations due to disease outbreak, pulling out and losing military ground the First Battalion of the King’s Africa Rifles had gained, would definitely be a “step backwards” from the viewpoint of the British colonial administrators.
Despite the threats and upon getting intelligence reports and news of influenza outbreaks that devastated Britain, Sierra Leone and South Africa in September 1918, the then acting Governor and Commander-in-Chief, Sir H. L. Duff, continued military operations and sped up the movement of troops across the country.[18] To respond to the spread of smallpox and bubonic plague, the acting Governor established infectious disease health centres near war locations, trade routes and communication lines.[19] The colonial government consequently extended its medical work creating new hospitals and by increasing the number of doctors and nurses to look after the soldiers and human porters during the war.[20] Despite these services, it was not clear how much the Governor had prepared for the coming of influenza outbreak, although he knew of the outbreak of influenza and its devastating impacts in Sierra Leone where it first appeared in Africa.[21] Records on the outbreak of influenza, gathered from the report dispatched to the Colonial Office in London from a Medical Officer of Nyasaland, 14 February 1919, suggests information and news about the spread of the disease was received by Nyasaland Protectorate at the beginning of September 1918.[22] The nation newspaper ran an article on the 17 October, 1918, for example, warning that Spanish influenza was fast spreading throughout Africa, but, in what provide to be the final weeks of the war, the governor simply could not undertake remedial measures immediately.[23]
The governor in Sierra Leone where influenza outbreak was virulent and dangerous also admitted that he failed to take precautionary measures to quarantine the warship vessel at the harbour because sanitary affairs of warships lied outside civil control and influenza was not a notifiable disease.[24] In his correspondence to the Secretary of State at Downing Street, the Governor Sierra Leone admitted the lost opportunity to prevent influenza outbreak from spreading had the vessel been quarantined much earlier.[25] The lack of signalling earlier warning about influenza angered most local inhabitants, who felt betrayed and cheated.
Diffusion of Pandemic Influenza: 1918-1920
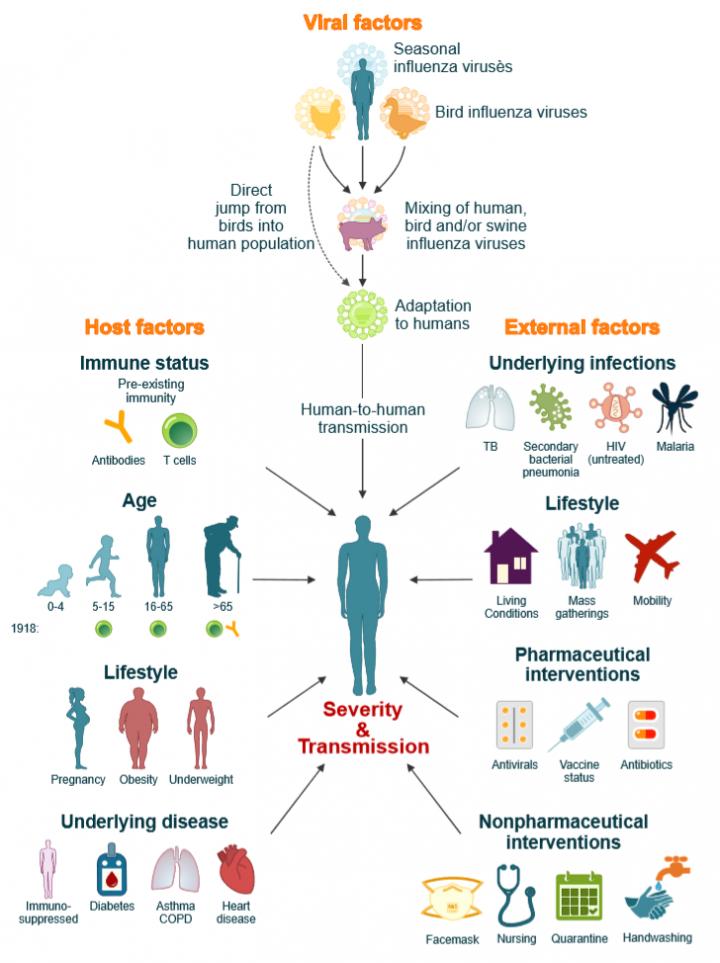
The spread of the influenza epidemic, including its consequences, was relatively similar throughout Africa as observed by many commentators.[26]Influenza came to Africa in three waves between August 1918 and January 1919. The first wave of influenza pandemic penetrated Africa through ports and harbours and made its way into the interior facilitated more by communication routes, drizzling weather, poor sanitation and the chaos following the great World War One. As a growing number of historians have recognised, the disease was introduced to Africa in a series of events. The first appearance of influenza in Africa was observed in Sierra Leone. On 15 August 1918 the HMS Mantua arrived in Freetown harbour with a large number of cases of Spanish influenza on board.[27] Pandemic influenza into the colony of Nyasaland was however introduced from the Union of South Africa. The earliest outbreak in the Union of South Africa occurred in the vicinity of the harbour area in Durban on 14 September 1918.[28]It spread to the central Rand area, where numerous cases were observed around the 18 September, chiefly among the natives working in mines.[29]
The cases of influenza in the Union of South Africa were predominantly mild, causing low mortality.[30]In October, however, the character of the disease in the Union of South Africa altered; it turned more severe and caused high mortality among the population. On 18 October, Salisbury (now Harare) reported the presence of influenza in the capital, and as a result Nyasaland immediately took action by prohibiting the return of its sick troops from the Union of South Africa through Southern Rhodesia. On 20 October, the disease was reported in Beira, Portuguese East Africa (Mozambique), and on 21 October, severe cases among local people were reported at Chinde (Mozambique).[31] Between 21 and 27 October, several cases were discovered among labourers on river boats and a railway line at Chindio (Mozambique). Subsequently, on 31 October, 1918 the colonial government issued a statement in the newspaper on how the general public should respond to the disease outbreak.
“Every case is to be reported at once to the nearest medical officer and Europeans to inform all the natives under their control, call meetings of all the headmen of their districts and explain the matter to them and tell them to warn every village as to the nature of the disease and what to do when it comes.”[32]
Figure 1 (below) illustrates the spread of influenza in Nyasaland. According to the register of correspondence, the first case in Nyasaland was declared on 1 November.[33] The virus penetrated Port Herald (now Nsanje) between 1 and 5 November, arriving from the terminus of the Shire Highland Railways in Portuguese East Africa. From there, it spread into the interior of the Protectorate, following the same lines of communication and movement as the troops on Lake Nyasa, and along rivers and roads.[34] Within a few days, on 9 November despite sanitary officials at Port Herald closing the border to prevent further transmission from Portuguese East Africa, influenza cases had been identified in Limbe and Blantyre.[35] From Blantyre, influenza spread northwards, following roads and the course of Lake Nyasa, to reach Zomba, the capital of Nyasaland, on 18 November. There is a controversy as to when influenza actually appeared in Zomba, although the capital is believed to have been affected much earlier than officially reported. For example, a telegram from the Governor of Nyasaland to the Secretary of State for the Colonies, reported a considerable increase in influenza cases by 13 November. A telegram reported that over 1000 people including 285 Europeans were hospitalized in Zomba due to influenza by 13 November. This suggests that the disease had reached the capital before 18 November.[36]
The disease swept through the protectorate in a matter of days. Between the end of November, 1918 and early February, 1919, the entire West Shire districts in the north of the colony were affected. The outbreak arrived in towns from more than one source such as roads, boats and rails. Towns such as Vua and Karonga are believed to have been infected much earlier on the basis of other evidence.[37]
Accurate information about the spread of the disease in most districts is difficult to obtain as local people who suspected infection hid serious cases to avoid racial segregation, discrimination and unpredictable actions from the colonial administrators.[38]Local people feared that once identified as having the disease, they would be separated away from their families and kept in isolation camps, and their dwelling huts destroyed if deemed unsanitary.[39]
Mortality from Pandemic Influenza
The influenza pandemic of 1918-20 is acknowledged as a major public health problem in Nyasaland. Although no accurate mortality statistics are available, some data exist. For example, the official mortality rate was reported as 117 per 1000 among indigenous people, among Europeans it was 47 per 1000 while for the Indians it was 147 per 1000.[40]Table 1 is return of cases, deaths and percentages of case mortality of the Europeans, Indians and indigenous African populations hospitalised in government hospitals. In his official despatch, the acting governor of Nyasaland estimated that only 1769 had died from influenza, including Africans, Europeans and Indians.[41] This figure, however, is not for the entire pandemic period and perhaps only covers the reporting period ending 31 December 2018. Influenza in Nyasaland is believed to have been sporadic with a few cases continuing to be recorded in February, 1920 in Karonga. In addition, the reported number of deaths excludes returns from non-government hospitals, many of which were ran by the missionaries. Missionary hospitals constituted a large source of incidence and mortality data thus attracting colonial doctors to approach mission doctors for information regarding key information on deaths, births and status of diseases especially in areas of the protectorate where few government doctors were posted.[42]
Although mortality data are scanty and unreliable, but judging from the correspondence records reaching the Chief Medical Officer, as many as 120, 000 or more may have died in the entire country. Utilising an approximate growth rate of 3.9% between 1911 and 1917 which I calculated using the formula PGR = P(t) – P(t0)/(P(t0) * (t – t0)) where PGR is growth/decay rate, P(t0) is the population in 1911, P(t0) is population in 1917 and t – t0 is difference in years between 1911 and 1917. In 1911 and 1917, official population was 967,183 and 1,227,442 respectively.[43] Further utilising a reported native death rate of 11.7% and using the exponential growth/decay formula x(t) = x0 × (1 + r) t, I calculated the total population ending February 2020 using a decay growth rate of -7.8%. In the formula x(t) is the value at time t, x0 is the initial value at time t=0, r is the growth rate when r>0 or decay rate when r<0, in percent and t is the time in discrete intervals and selected time units. I calculated the decay rate by subtracting growth rate (3.9%) from death rate (11.7%). Between December 2017 and February 2020, the total population decreased from 1,227,442 to 1,104,467 suggesting 122, 975 native population had died. This figure is similar to those suggested for other African countries by Johnson and Mueller.[44]
According to the officials reports the total native population in 1917 was 1,227,442 and this dropped to 1,215,976 in 1918, a reduction of 11,466.[45] This drop would have been for the year ending 31 December 2018 covering 3 months of the outbreak at most. Aggregated figures are difficult to obtain but there is no doubt that even the figure I have suggested here is far from reality since many people affected by pandemic influenza where located in remote areas of the country where they remained untreated and many deaths occurred without being reported to the authorities. Even the Acting Governor, in his covering despatch about the state of the epidemic to his counterpart in London, wrote: “It is important to note that the statistics despatched are far from being an exhaustive record of the epidemic, since scores of thousands of cases have occurred in outlying native villages.”[46] This was also supported by remarks made by a medical officer that “the absence of vital statistical returns of the general population of the protectorate can as well be seen as limited value to public health.”[47]
While it is impossible to ascertain precisely the number of people who died from the disease from the 1918-20 pandemic, it is evident that there was a severe demographic effect on population. A high death rate and low fertility rate during the pandemic period decreased the total population in 1920 and the subsequent growth of the population thereafter. Deaths were much higher among young male but also high among pregnant women thus offering a tentative explanation why there was a reduction in birth in 1920s.[48] Annual report for Nyasaland ending 2018-19 show that there were more women (664,400) than men (551,600) within the local population.[49] Since young men who were possibly in the Amy formed a large cohort of those that died and those that were left perhaps were young enough to marry meant that women had to wait for marriages than normal. This either affected the marriage patterns or the fertility rate.
As far as large differences in mortality rates between the Europeans and local people is concerned beg a number of epidemiological explanations. Just as the Medical Officer serving the colonial administrator observed “It was apparently difficult to do much for the indigenous population, to whom the disease was a complete novelty”.[50] The living conditions of indigenous people provide a more compelling reason especially that the sanitary conditions for indigenous people were much lower than Europeans, with many lacking access to sanitary latrines, cisterns or tanks and rainwater was often used for drinking and cooking purposes.[51] Although influenza is airborne, there is potential risk of possible direct inoculation by the contaminated environment. The sanitary department was still unorganised, running on insufficient funds to extend necessary measures and maintain trained indigenous sanitary inspectors.[52] Overcrowding among the indigenous people plus troops in close quarters if no demobilisation and labourers in labor lines many have been other potential factors that facilitated high mortality rates.
Responses to the Pandemic
Apart from deaths, influenza directly affected those who survived. The disease left orphans without anyone to help them. It is impossible to ascertain precisely the number of children who were orphaned or deserted due to lack of records. However, there are reports that orphaned and abandoned children took shelter at Churches with the majority African orphans absorbed by extended families and networks.[53] The pandemic further caused great personal suffering and disruption of social and economic activities throughout the colony. It affected the collection of taxes owing to large defaulters. As Musambachime has shown significant reduction in the collection of taxes reached well below 22 per cent in 1918 compared to previous non-pandemic tax year periods.[54]The tax defaulters are believed to have been young men between 15-40 years who either died or ran away from tax obligations including employment thereby creating labour shortages and economic disruptions in agriculture, transport, export and health.
Influenza outbreak steered panic and fear among local people that it affected crop production since subsistence farmers abandoned their farms by fleeing areas that had the disease. Ohadike also describes how millions of the city dwellers in Nigeria fled to remote villages, while the villagers themselves escaped into the bush and hid themselves in their farmhouses.[55] This pattern of movement directly affected the ploughing and other activities in preparation for planting season that coincided with the peak of the epidemic. Meanwhile there was a shift of responsibilities from farming and grazing cattle to looking after the welfare of the sick. This eventually compounded poverty and brought drought, which heralded future famine and triggered further movement of people in the north of the protectorate to cross into Northern Rhodesia, now Zambia in search for food.[56]Elllison noted how influenza caused famine due to demographic disaster, which was felt at the time when the onset of rains was not met by enthusiastic planters, as many farmers were ill and dying. Subsequent rounds of epidemic waves also disrupted the vital work of weeding for those who had planted. Farm labour collapsed and crops that were ready for harvest stood abandoned in the fields. Increased theft in farms was observed in many parts of Africa in order to survive. Also limited travel to markets or funerals meant people stayed in their own homes to eat their reserves without stocking up but just hoping for the best.
Little is known whether there was a change in the staple foods due to food shortages or change in gender roles due to women being sick in Nyasaland. However, in the Gold Coast, for example, change in gender roles was observed since many women were sick and men had to pound seeds to remove husks and prepare meals.[57]Change in cultural practices was also noted in Nigeria where staple foods changed. Ohadike describes how cassava, once rejected as a staple, became accepted in the aftermath of the pandemic.[58] Due to the frequency in the occurrence of deaths and rapid movements of people, it become very difficult for families to arrange burial ceremonies in manner there were practised in Nyasaland. Burial rituals significantly changed with reports that those that were buried were either buried without ritual performances or cerebrations by dancing or killing a cow. The dead bodies could no longer be cleaned or kept in the house overnight before burial. In many cases, the bodies were left abandoned or left to rot along the road.